Weight Loss Surgery
ABOUT OBESITY
OBESITY AND MORBID OBESITY
Obese:
Body Mass Index (BMI) of 26 or greater. (BMI=kg/m2).
Morbidly Obese:
Body Mass Index (BMI) of 37.5 or greater (Roughly equivalent to 35 kg. over your ideal body weight).
The Clinical Guidelines For Consideration Are:
• 35 kg. or more above ideal body weight or a BMI of 37.5 or greater.
• BMI of 32.5 or greater with one or more obesity related health conditions.
Other Considerations:
• History of documented dietary weight loss attempts.
• Lifelong commitment to follow-up care and extensive dietary, exercise and medical guidelines.
• Psychological evaluation.
OBESITY CAN RUIN YOUR HEALTH
Obesity is the root cause of some of the common diseases as follows:
Type 2 diabetes:
People with obesity develop a resistance to the insulin that regulates blood sugar levels. Over a long period, high blood sugar can cause serious damage to the body.
High blood pressure/heart disease:
Excess body weight over-burdens the heart to function properly. The resulting hypertension (high blood pressure) can result in strokes (brain hemorrhage), significant heart and kidney damage.
Osteoarthritis of weight-bearing joints:
The additional weight placed on joints, particularly knees and hips, results in rapid wear and tear, along with pain caused by inflammation.
Sleep apnea/respiratory problems:
Fat deposits in the tongue and neck can cause intermittent obstruction of the air passage leading to interrupted sleep. The resulting loss of sleep often results in daytime drowsiness and headaches.
Gastroesophageal reflux/heartburn:
Obese people are susceptible to acid escaping into the esophagus through a weak or overloaded valve at the top of the stomach.
Depression:
Repeated failure with dieting, disapproval from family and friends, sneers and remarks from strangers, constant struggle with fat puts immense mental strain, pushing patients into depression.
Infertility:
The inability or diminished ability to produce offspring.
Fatty liver or hepatic lipidosis (steatosis):
Fatty liver disease is the accumulation of fat in liver cells. The greater the percentage of fat in the liver, the greater the risk of developing liver inflammation, fibrosis, or cirrhosis (moderate or severe scarring of the liver).
Others:
Other problems include swollen legs/skin ulcers, urinary stress incontinence, menstrual irregularities, lower extremity venous stasis, Idiopathic intracranial hypertension (IIH), dyslipidemia (lipid metabolism abnormalities), pulmonary embolus and cancer.
BARIATRIC / WEIGHT LOSS SURGERY
"Weight loss surgery is not a cosmetic surgery"National Institute of Health consensus conference has concluded that surgery is the only effective treatment for long-term and sustained weight loss which results in improvement and/or resolution of co morbid conditions, improved quality of life and self-esteem, and increase in longevity.
The most common question people ask is - what is Obesity surgery? ….. is it same as liposuction?.....
No! Liposuction is a surface surgery performed to remove extra unwanted fat from different part of body, this is basically a surgery for body sculpturing not weight loss, where as obesity surgery (bariatric Surgery) gives options for the treatment of this disease evolved into three categories, restrictive procedures, eg. Gastric band, sleeve gastrectomy, malabsorptive procedures, eg. Biliopancreatic diversion with or without duodenal switch, and combined procedures, eg. Roux-en-Y-gastric bypass (RYGB). Hence, selection of the procedure has to be individualized based on the age, BMI, presence or absence of co morbidities, patient's preference and compliance, surgeons experience etc. However, the experience of the bariatric surgeon is the most crucial in selecting the right procedure for an individual.
ANATOMY OF THE DIGESTIVE SYSTEM
Starting from the top we will explain the anatomy of the digestive system to understand how the operation works:
- Mouth : Entry point for food; teeth and tongue chew food and move it to the back of the throat for swallowing. The enzyme amylase starts digestion of starches and sugars (carbohydrates). .
- Esophagus : Carries food to the stomach. It has no digestive function.
- Stomach : Holds food and mixes it with acid and saliva. It has no absorptive function.
- Pylorus : The valve that controls the emptying of the stomach. It helps to prevent "dumping syndrome".
- Small Bowel : This tube, 5 meters (15-30 feet) in length, lies in between the pylorus and the large bowel (the colon). 95% of digestion is carried out here and it is the most important part of the digestive system. It is divided in 3 parts:
- Duodenum : Two feet long (60 cm). Bile from the liver and pancreatic enzymes (the digestive juices) enters this segment.
- Jejunum : The middle portion of the small bowel.
- Ileum : The lower portion.
The jejunum and ileum are the sections where carbohydrates, proteins and fats are absorbed, as well as vitamins and minerals. Iron and Calcium are absorbed in the duodenum. - Large bowel : Starts at the end of the small bowel. Its main function is absorption of water and holding the stools. Nutrients are not absorbed here. The appendix joins the bowel at its beginning.
- Liver : Nutrients absorbed from the small bowel go to the liver via the portal veins. Secretes the bile necessary for fat digestion.
- Pancreas : Secretes the enzymes necessary to digest carbohydrates, proteins and fats.
HOW DIGESTION WORKS ?
Digestion stars in the mouth with saliva's amylase. Food travels to the stomach where it is held, and mixed with acid. It starts to break down here. Stomach emptying is regulated by the pylorus. Digestion and absorption happen in the small bowel when food is acted upon by bile from the liver and pancreatic enzymes. Water is absorbed in the colon and waste is excreted through the rectum.
WEIGHT LOSS SURGERY PROCEDURES
There are two basic mechanisms of weight loss surgery.
- Restrictive procedures decrease food intake by creating a small upper stomach pouch to limit food intake.
- Malabsorptive procedures alter digestion, thus causing the food to be properly digested and completely absorbed. There are several procedures that combine the restrictive and malabsorptive mechanisms of weight loss surgery.
HOW EFFECTIVE IS BARIATRIC SURGERY?
"The only way you can truly get more out of life for yourself is to give part of yourself away."
The actual weight a patient will lose after the operation depends upon several factors. These include:
- Patient's Age
- Weight Before Surgery
- Overall Condition of Patient's Health
- Surgical Procedure
- Ability to Exercise
- Commitment to Maintaining Dietary Guidelines and other Follow-up Care
- Motivation of Patient and Cooperation of Family, Friends and Associates
A recent study established the following criteria for successful bariatric surgery: "the ability to achieve and maintain loss of at least 50 percent of excess body weight without having significant adverse effects".
Clinical studies show that, following surgery, most patients lose weight rapidly and continue to do so until 18 to 24 months after the procedure. Patients may lose 30 to 50 percent of their excess weight in the first six months, and 77 percent of excess weight as early as 12 months after surgery. Many patients with Type II Diabetes, while showing less overall excess weight loss, have demonstrated excellent resolution of their diabetic condition, to the point of having little or no need for continuing medication.
A comprehensive clinical review of bariatric surgery data showed that patients who underwent a bariatric surgical procedure experienced complete resolution or improvement of their co-morbid conditions including diabetes, hyperlipidemia, hypertension, and obstructive sleep apnea etc.
There are five widely performed procedures that can be employed to lose or maintain weight.
- Laparoscopic Sleeve Gastrectomy (LSG)
- Laparoscopic Roux en Y Gastric Bypass (LGB)
- Laparascopic Adjustable Gastric Banding (LAGB)
- Laparoscopic Gastric Imbrication
- Laparoscopic Biliopancreatic Diversion with Duodenal Switch
Sleeve Gastrectomy
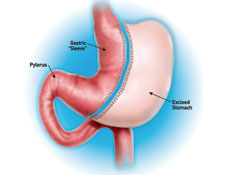
Laparoscopic sleeve gastrectomy (LSG) is a new bariatric technique, which has a unique feature: it combines a satisfying gastric restriction with appetite suppression.
In other words, LSG has a physiological advantage over other restrictive procedures such as gastric banding. Furthermore, in LSG no foreign material is implanted avoiding complications such as migration, erosion and infection.
The risk of peptic ulcer or dumping is low, while absorption of nutrients and orally administered drugs are not altered as may transpire after gastric by-pass. LSG provides substantial weight loss and resolution of co morbidities to 3-5 years follow-up. Comparative data demonstrate percent EBWL at 1 year superior to AGB and approaching that of gastric by-pass.
- No silicone implants.
- Great appetite suppression.
- Lower risk of peptic ulcer.
- No dumping.
- No vitamin or drugs malabsorption.
- It does not impair patient's dietary habits.
- Better weight loss than gastric banding.
- No important late complications.
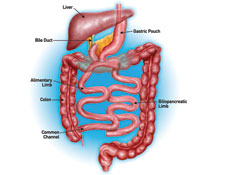
Roux en Y Gastric Bypass
Procedure Type : Combined Restrictive / Malabsorptive
Description :
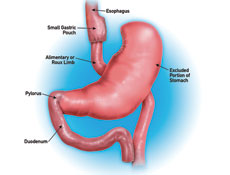
- Stapling is used to create a small, upper stomach pouch which restricts the amount of food to be consumed.
- A portion of small bowel is bypassed thus delaying food from mixing with digestive juices to avoid complete calorie absorption.
Result :
- Average of 77% of excess body weight loss one year after surgery.
- Studies show that after 10 to 14 years, patients have maintained 60% of excess body weight loss . Study of 500 patients showed that 96% of certain associated health conditions studied were improved or resolved, including back pain, sleep apnea, high blood pressure, Type II diabetes and depression.
- In most cases patients report an early sense of fullness, combined with a sense of satisfaction, that reduces the desire to eat.
Lap Adjustable Gastric Banding
Procedure Type : Restrictive
Description :
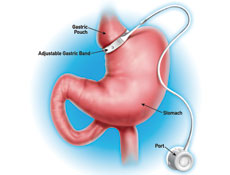
- A band is placed around the upper most part of the stomach separating the stomach into one small and one large portion.
- Band can be adjusted to increase or decrease restriction.
- Surgery can be reversed.
- Digestion and absorption is normal.
Result :
In a U.S. study, the mean weight loss at three years after surgery was 36.2% of excess weight.
Laparoscopic Gastric Imbrication
LAPAROSCOPIC GASTRIC IMBRICATION (LGI) is an innovative restrictive technique for the treatment of morbid obesity. This operation, which initially introduced by Prof. Talebpour* from Tehran University, may be considered as an advancement of the well-known sleeve gastrectomy and it is carried out with the use of pure non-absorbable surgical sutures.
In LGI the gastric capacity is diminished without gastrectomy or foreign implants. Due to the lack of gastric strictures LGI does not cause any food intolerance nor impair patient's dietary habits. The resultant weight loss is comparable or better than gastric banding (55-60% EWL), but with LGI the loss of weight appears more rapidly. Overall, in comparison to the other modern restrictive bariatric techniques the unique advantages of the LGI are:
- Minimal risk of early of late complications.
- It does not impair patient's dietary habits.
- The operation is reversible. Gastric sutures withdrawal will get the stomach back to its normal form.
Preliminary results encouraged us to adopt this operation as better bariatric solution for lower BMI's (35-45 Kg/m2) in the stand of gastric banding
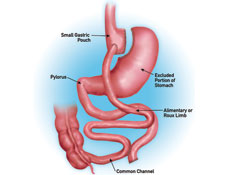
Biliopancreatic Diversion with Duodenal Switch
Procedure Type : Malabsorptive
Description :
- Combines a lower level of restriction with a high degree of malabsorption.
- Stapling is used to create a sleeve of stomach retaining the natural stomach outlet.
- The majority of the small intestine is bypassed causing nearly complete malabsorption of food contents.
Result :
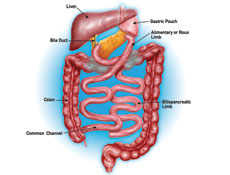
- Patients have achieved excess weight loss of 74% at one year, 78% at two years, 81% at three years, 84% at four years and 91% at five years.
- Provides less restriction of food consumed than other procedures discussed.
- Provides highest levels of malabsorption.